Hello all again. We are getting so much closer to our goal to get our senior residents to our national conference in May. Thank you all for your support. Please take a look at our fundraising page after reading our next post. As I write this, we are 42% of the way to our goal! Please help up get all the way there!
—————————————————————————————————————————
In the third and final installment of playing the “long defeat,” we get to discuss our biggest failure yet. The young, beautiful and courageous Hana from Bahir Dar. Featured in my most embarrassing post of this blog, back in the fall I was introduced to an 18 year old dramatically suffering from the “long defeat.”
In the spring of 2018, Hana was diagnosed with acute kidney injury following an aggressive episode of food poisoning. While in renal failure, she developed respiratory distress and required intubation. After a prolong period of intubation, she was extubated only to have developed subglottic stenosis from the endotracheal tube plastic.
The capillary blood pressure (the amount of pressure needed to occlude blood flow) in the tracheal mucosa is around 30 mm of mercury. When too much air is slammed into the balloon of the endotracheal tube, it can easily surpass this capillary blood pressure. When this happens, even for a short while, the mucosa dies, falls off and the body replaces it with scar tissue. When this occurs concentrically in the trachea, you end up with tracheal stenosis.
When you extubate someone with tracheal stenosis there can be sudden or delayed respiratory distress. After securing the airway, the correct initial management is bronchoscopy and endoscopic management of various sorts to re-open the airway and minimize scar tissue. Often this is difficult and sometimes impossible which will require a bypass of the narrowing and a tracheostomy. This is not the practice in even the best hospitals in Ethiopia. Patients are trached allowing the stenosis superiorly to develop as much as it wants.
Hana wasn’t given the chance to fight this. After her airway distress, a tracheostomy was placed and less than a week later, the general surgeon at her hospital decided to perform the heroic procedure of cutting out the stenotic segment and then putting the trachea back together. This resection and anastomosis can be simple, but often isn’t, wrought with life-threatening complications.
Within weeks of her surgery, she was back in the hospital with respiratory distress requiring a new tracheostomy. By this point, her father had sold his house and every other valuable he owned to pay for the mounting medical bills. Hana dropped out of school and was certainly isolated and depressed. Fast forward 6 months when a call from an official in the Ministry of Health gets to Yilkal requesting us to help Hana. A trip in the fall to her home town in Bahir Dar was the focus of a previous post.
After deciding to fly her to Mekelle for a formal bronchoscopy it became clear that fixing her severely injured trachea may not be possible. She suffered from chronic airway inflammation and reflux not to mention that her oropharynx was so crowded, she would probably suffer from obstructive sleep apnea if she were able to breathe through her larynx. Thus, while she visited in January and we discovered a thick 99% stenosis of the proximal trachea up to the level of the cricoid, I took the opportunity to maximize her airway. I placed her on daily dual reflux medication and performed a tonsillectomy to open the way for future air to travel.
We sent her back to Bahir Dar to wait for the right moment. Contemplating a revision tracheal resection and anastomosis on an 18 year old with poor anatomy and inflamed mucosa, I knew that failure was a real possibility. To maximize our changes, I planned the surgery to coincide with the visit from a stellar head and neck surgeon, Terry Day.
Hana and her desperate father understood the consequences of failing again, but there was no other option in their minds. And I was ready to fail with them. The politician in the Ministry of Health used his own money to fly Hana and her father up to Mekelle for the procedure.
Our entire team sat down with Hana and her father to discuss the procedure. I never go into a surgery thinking I will fail, but I am realistic. I always hope to win but understand I can’t every time. I wanted nothing more than to cure Hana.
An hour into the procedure we had the trachea isolated and it was a mess. Scar everywhere, surgical planes completely disrupted and cartilage in places they shouldn’t be. The resection of 3cm of scared trachea was simple enough. The distal trachea was freed from any tissue we could reach and the proximal was released by cutting a group of muscles around the hyoid. With the innominate artery in the breeze, the two ends of trachea met each other with more resistance than I would ever like.
With the repair completed and the trachea stented with an endotracheal tube, we brought here to the ICU for perhaps the longest 7 days of our lives.
I had prepared our team, Hana and the ICU team for this postoperative management. She was to be wide awake in the ICU, on the vent while the endotracheal tube stented across her new airway. This must have been impossible for her, but Hana greeted us every day with a smile and a thumbs up.

7 days of sitting in the room filled with dying patients, ambient light and never-ending beeps and alarms. ICU psychosis is a real thing and as reality begins to slip, you need all the help you can to return to it. In Hana’s case, it was movies. Our residents helped me figure out how to download movies onto a data card for her phone and I prescribed her whatever movie she wanted, downloaded it, and made daily deliveries.

By the end of the 7 days, it was all smiles and no complications. We put everything in order for her to be extubated that morning. Right when I arrived to bedside, she had a massive coughing fit and I saw her neck inflate with each cough. Like someone had attached a tire pump and was intentionally inflating her wound.
I palpated her neck and without saying a word, quietly walked away. Inside, I was ruined but maintained an external shell for the sake of Hana. Our surgery had failed and a hole somewhere in the trachea was leaking free air into the neck. If it continued, it could dissect all the way from scalp to toes, eventually causing a tension pneumothorax and cardiac arrest. There was no other option than to mobilize back to the operating room.
After explaining our failure to Hana and her father, I rolled with her back to the operating room. I didn’t know what I was going to find, but I knew it wasn’t going to be good.
Failure is medicine. When treating complicated patients, you often transition through various failures until you find the perfect combination to maintain some new steady state of normal. A successful surgeon is someone who can predict what failures will happen and put in place measures to minimize their effect. And, when unpredicted failures occur a successful surgeon will adapt, persist and remain patient.
Hana was losing her chance at being normal, at being able to speak and at being reaccepted back into social society. When we opened the neck, I saw this reality. The trachea never really healed. The sutures had ripped through and the anterior tracheal wall was falling apart. With the anterior wall a mess, there was no repairing this. An adaptation was the only option.
With the proximal subglottic area healthy, I decided to stage her recovery. Reinforce the trachea, replace the trach and to stent the upper segment with a cut endotracheal tube. In a couple weeks I would remove the stent and dilate the proximal airway to keep it open. Eventually, if we are able to keep the proximal airway open, we would decannulate and allow her body to heal the anterior tracheal wall defect slowly over time. If she couldn’t heal completely, I’d patch the hole with a small piece of cartilage.

We had failed. But we did it together. I will continue to pour my time and resources into her because we are in this long fight against failure and we will always work towards winning.
To add insult to injury, Hana turned 19 in our hospital just days after her failure. I was out of town, so I asked the residents to blow up some balloons I had on my desk and to give her a lollipop I had left over from a mission trip. What they ended up doing brought tears to my eyes. In the wake of certain lifelong pain and social ostracization, stuck between the now-familiar walls of her overcrowded hospital room, our team threw her the most amazing birthday party.
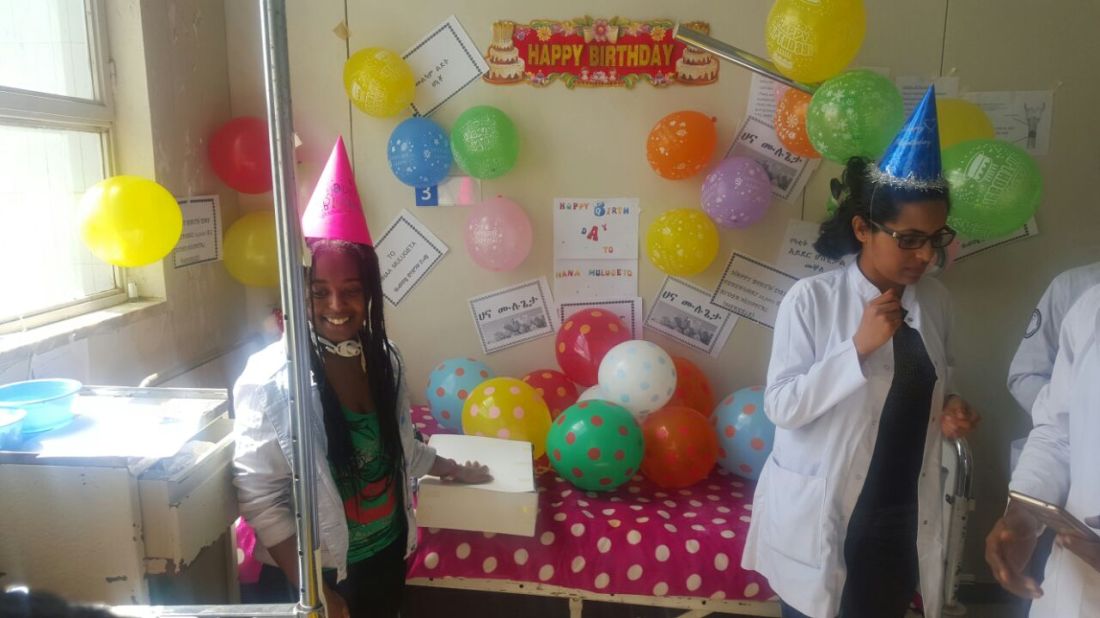



Even our young chondrosarcoma patient joined and enjoyed gumming the cake with her newly created oral obturator. Our newborn with bilateral choanal atresia came by, blissfully unaware of the stents that now kept her alive and thriving.
At that moment I was actually in Bahir Dar visiting with Hana’s brother who stopped by to meet me. Him and I shared in the joint sensation of happiness for Hana as we thumbed through the pictures sent by my residents. For, in those moments, her life probably seemed normal. Perhaps for the first time in the past year.
Her only chance at keeping that proximal segment open if frequent follow up. Thus, I will be traveling to Bahir Dar every couple of weeks to look at her airway and dilating as needed. This is far from over and I’m looking forward to my visits to Bahir Dar to continue the fight. And at the very least to see Hana’s smiling face and say hello to her ever-accumulating collection of stuffed animals.

Thank you all again for following along with us. Help our residents get to their conference in the US. Everyone tiny donation counts!





Ohhhhh Professor Joshua! no more words !i wish to mention /explain more about you but i failed ! unfortunately am not rich in words !am not lucky to use this opportunity to show you my gratitude,respect,appreciation and love etc !i know as you stated earlier in your post i lost many but here after i will never be sad because i have seen everything what you are trying to do. you did it all to save my daughter life and make her life better as far as you can the other thing remains up to Almighty God ! am not flattering i swore ! you are so generous & kind for me ! wow ! still i would say sorry not to be rich in words, not able to explain you in better words!because you are more than what i explain you !
Thanks again and again ! God bless you ! hope who knows one day i will be rich in such words and will be able to explain you more and more ! finally please pass same appreciation to Dr yilkal & Dr zerihun (both should take the lion share) and your ENT staff. am glad know you in those desperate days
yours sincerely Mulugeta (Hana’s father)
LikeLike