Allow me to begin this post with some lamenting. Although I’ve somehow made it through 3 weeks relatively unscathed, I always seem to be in some state of disarray. Aside from the ever-present foodborne illnesses, my American viral immunity that I’ve been working on all my life (from parents bringing me home colds to my medical training exposure), does not apparently cover the Ethiopian common cold. Add with that a near 72 hour stretch of power blackout at my house, and you have a pretty ornery, spoiled American 30-somthin year old. Nevertheless, I’d like to battle past my annoying copious clear rhinorrhea and speak about my amazing week.
AH! And with that, the light above me flickers to life!…….
Now I’m back, armed with every device charging next to me and a fresh espresso, seasoned with a surprisingly delicious powdered milk and sugar. Forget my entire first paragraph, life is so good. This post will be mostly medical and I’ll place another for my weekend adventure.
The week featured an onslaught of new and complicating diseases, some of which, I really need your help with! Also, my role as an educator expanded into other departments and to the medical students. I am loving my role at this institution and its only 3 weeks in. I can’t wait to see where this goes.
Lets start with the most dramatic case first. By this time, we all know the gentleman with the large ulcerating right neck mass. He, unfortunately, has had a very serious turn for the worse and I want to re-present the case from the beginning, here, to illicit thoughts from you. People that read this blog are some of the smartest people I know and represent basically the entire spectrum of science from molecular biology, to infectious disease, to pathology, to super sub-specialized surgery. I’ve already reached out to a lot of you about these cases, but why not use this as a crowdsourcing forum. I’ll open up a way to comment and respond to this posting, but please feel free to call me on WhatsApp or e-mail me at josh.wiedermann@gmail.com if you have any bright ideas.
Ok… This otherwise healthy 38-year-old originally presented to this hospital about 3 months ago with a right neck mass. On that initial evaluation, he was felt to have bilateral palpable cervical lymphadenopathy and because he lacked any other symptoms (according to the hard written record), he was sent for an MRI. Although he obtained it 3 months ago, he was then lost to follow up and decided to treat the rapidly enlarging neck mass with a tropical homeopathic drug (I have no idea what it was). He then presented to us 2 weeks ago with the large right ulcerating neck mass. After reviewing the two-month old MRI (posted here), all I could really discern from the motion artifact-laden pictures was that he had diffuse, bilateral homogenously enhancing lymph nodes without central necrosis and that the one lateral to his right sternocleidomastoid muscle ruptured. Since he presented on a Friday, the original plan was to try to find a heme/oncologist (a medicine doctor that is interested in these subjects) and, then on Monday come up with a longitudinal plan.

Well, on arriving to the hospital Monday, we found him tripoding in respiratory distress with new facial nerve palsy. I’ve never seen anything move this quickly, but I’ve also never seen anything this aggressive before either. We took him for an emergent awake trach, wound debridement and biopsy. The ulcerating wound was not overly necrotic. Most areas I probed were bleeding and I could still feel abnormal tissue. I took biopsies of the abnormal tissue and committed my first mistake of his care. I submitted the specimen fresh (instead of fixed in formalin) because I had been taught to send material suspicious for lymphoma in this way to allow for flow cytometry. Well, there isn’t flow here and the pathologists had a difficult time fixing the specimen and their final reports read “indeterminate.” Immediately following the trach, he was placed on ceftriaxone and metronidazole (the standard cocktail here which I’m beginning to distrust), steroids, given wound care and a nutrition consult from my wonderful friend, Judith. He dramatically improved over the next 48 hours, the various masses in his neck seemed to dissolve and he was just left with a trach, a paralyzed right face, and a huge neck ulcer.
I spent the following days this week having discussions with pathology (I even went down there to look at the slides and take pictures as best as I could), the medicine doctor that was going to take the case, and watching closely over the patient. He was well, in good spirits, eating, phonating and without any signs of illness. We stopped his steroids after 5 days, but kept his ceftri and metro. The pathology to me showed very abnormal cells with abundant pleomorphic nuclei with mitotic figures even I could find. This was unfortunately in a bed of necrosis and poorly fixed specimen so no definitive diagnoses could be made.

Thus, before the internist would treat, shed want another biopsy. I returned to the patient to get a good repeat physical exam to see if I could find a leftover lymph node to biopsy. I couldn’t. They seemingly have melted away, which I have read and seen occurs sometimes in lymphoma. Nevertheless, this gave me a chance for a good look at his neck wound. Something had changed, seemingly overnight, as a black eschar now filled the bed of his ulcer rather than granulating tissue. I pulled gently, which caused pain. Since he was stable, looked well and we needed new pathologic specimen, I decided to set him up with a new CT with contrast to look for a place to biopsy and to re-assess his wound that I would eventually need to close with some type of tissue.
The result, as you can see, is whatever is more dramatic than dumbfounding. In a matter of days, his wound had silently necrosed though all lateral structures of his neck and was on, or 1mm away from his carotid artery. I sat there in the OPD, staring through these images over and over again, silent. Looking for evidence to convince me this was some type of ridiculously aggressive malignancy or necrotizing fasciitis. I was clinically stumped, but knew I had to return to the OR immediately to debride everything I could. His wound was filled with this sticky, foul smelling, necrotic mass, adherent to all deep structures. As I debrided, I took verbal account of structures that had been obliterated by this biologic nightmare. The dictation was for teaching, of course, but also to help me create a map of where vital structures would lie in this sea of unidentifiable tissue planes. The SCM, posterior belly of the digastric, the omohyoid, the lateral strap musculature, the submandibular gland, the tail of parotid, the internal jugular vein, the facial artery and vein…..all gone and lifted along with this necrotic mass I dissected free from the carotid sheath.
The carotid pulsations were obvious and emanated from a bed of necrotic tissue in its sheath. The thrombosed IJ sat just lateral. I could palpate the angle of the mandible, mastoid tip, transverse process of C1 and the thyroid cartilage all within the field. The necrotic debris, for the most part was removed apart from the focus on the carotid. I knew from my experience with squamous cell carcinoma that the carotid was one gentle dissection away from exploding in my face, so the necrosis I could see on the carotid itself was left in place.
Now the decision was, should I prophylactically sacrifice his carotid? I could make the basic assumption that there was a high likelihood that there would be a blow out. But, sacrificing the carotid now would put him at a serious risk for stroke. Not to mention that obtaining distal control here would require isolating the external and internal branches separately to prevent backflow if we ligated proximally. It wouldn’t be an easy surgical procedure. Being hemipelagic in Tigray may be worse than death. I wanted to have this discussion face to face with him so I decided damage control was best and woke him up. I sent the dead tissue for culture and anything that was semi-alive for path. I added fluconazole (the strongest antifungal we can get), vancomycin and meropenem. I instructed the residents how to do dressing changes over the weekend and to send me daily pictures. I’ll plan this face to face discussion on Monday and hopefully will have some micro or path to work with.
Interventional radiology doesn’t really exist for balloon occlusion studies or stenting. Vascular surgery gave us a blank stare and other than the plan I have laid out, I’m out of ideas.
Now, given the story and images, does anyone out there have any other recommendations? I’m all ears.
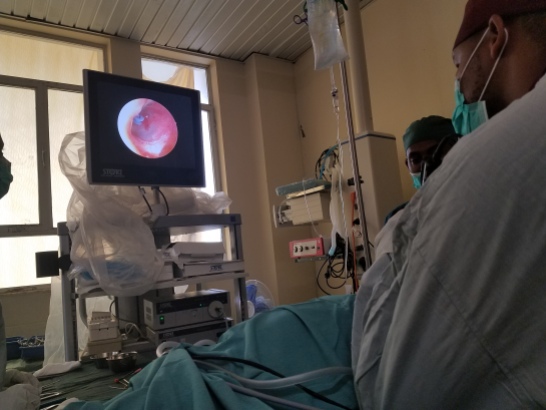
Lets move on to some of the happier times in the Hospital. I was honored to be asked to join in the OR with one of the more senior general surgeons for a pediatric (2yo) airway foreign body. The story I got was this child ate peanuts 1 month ago, choked and ever since has had a chronic cough and wheezing. A slam dunk FB story. The physicians here have a lot of pride in their education and skill, so I knew it was an honor to be invited into his OR. I went in with the mindset only to offer advice and technique tricks. I explained to him and the anesthesiology tech (oh, what I learned also is that all the anesthesiologists here at most have a master’s degree in the field. There is no requirement of a medical degree), that we would induce with halothane gas only and once calm and spontaneously breathing would perform the bronchoscopy. As they set up, I looked over the equipment. It was good. A 3,5 Storz ventilating bronchoscope, 4mm 30 degree (no zero) that was roughly the correct length and an optical forcepts that fit through the bronch. This was much better than I expected and should be plenty to do the job.
With everything ready, we induced and O2 sats remained in the high 90s with spontaneous breathing. On DL, however, he desaturates quickly and there was only time to anesthetize the cords. I borrow the stethoscope and appreciate significantly decreased breath sounds on the right. Looks like there actually is something down there. On the next DL, he struggles to get good exposure and the technique is labored. Eventually, he passes a suction and frank purulence returns. Great…
On the 3rd and 4th attempts, he tries to pass the 30 degree into the larynx but struggles. I can see he is trying to do this under direct view rather than using the projection from the endoscope. I mention the change in technique, but by this time, we have to bag the child and his stomach fills with air which we decompress. I make the bold move and ask to sit down. Now the basic technique is there, but the hesitation in execution for just those couple of seconds forces us to abandon the attempts. I wanted to show how just tiny changes in technique can buy you all the time you need. I sit down and can see my residents whip out their phones and I hear the sound of digital photos capturing. Some from behind me too. I ignore this, tell my plan to the anesthesiologist and execute. Just as I have done hundreds of times before I extend his head, open the mouth, insert the laryngoscope and move the tongue to the left while tracing the tongue base into the vallecula, establish a grade one view of the larynx, pass a suction and guide the endoscope into the trachea. Wading through some residual purulence, a white mass comes into view completely occluding the right mainstem, with its tip just proximal to the carina.
With a clear objective in hand, I remove the endoscope and bag mask. I ask the tech to assemble the bronch, which she clearly did not know how to do. So, with my left hand holding mask, my right pieced together the 3,5 bronch ready to ventilate and remove the right mainstem FB. On cue, I insert the bronchoscope and saturations are maintained…as long as I plug the 2 or 3 holes along the bronchoscopes various connections. I ask the general surgeon to grab the optical forceps which he gladly does. On the next cue, he inserts the opticals and grabs the FB tightly. I instruct to pull just to the tip of the bronch and then we will come out together. The glee in his voice gave me joy, keeping in mind that this was the most critical point of the procedure. Together, in harmony, we remove both instruments and out came a large peanut half (intact). It is quickly whisked away and as a photo shoot occurs behind me, I perform the final look and wake the patient up. Damage had certainly been done from the oils of the peanut, but after the purulence was removed, the right lung ventilated well. Airway FBs are one of my favorite procedures and I was elated and honored to be able to take part in this one.
After the child was in PACU, I went to see if I had damaged my relationship with the general surgeon by taking over his case. I really didn’t want to be hands-on, but it was the right thing to do. I thanked him for having me and encouraged him to do the same again. He seemed genuine when thanking me, but its hard for me to tell. Ethiopians are very polite and this relationship is one I want to keep. I’ll be sure to be on the lookout for ways to be useful to him in the future.
I’ve also taken a much bigger role in teaching this week. On Wednesday and Friday mornings, I gave hour-long lectures on diseases of the oropharynx and larynx to the medical students in their clinical years. It was in a large, dusty, stadium-style classroom, with a very nice flat screen set up which connected directly to my laptop. They say that this classroom has good enough WiFi connection to do teleconferences which might be interesting once I get Tumor Board up and running. The medical students were eager and excited. There were probably about 40 people in the class and 90% of their eyes were either on me or writing notes. Not a single cell phone was out. It was clear they were here to learn and I really enjoyed teaching them.
In the OR, I walked Seid, one of the R2s through an endoscopic myringotomy tube. A relatively simple procedure, but he executed it very well. Myself and all the residents sat down on Friday to start planning the academic additions to the program (Formal rounds, Morbidity and Mortality, Radiology Rounds, Tumor Board, Journal Club). I created them a word document “Inpatient List” that they will now keep updated and bring on rounds. I also showed them how I want notes completed before rounds are over so that everyone understands our plans for the patients. We all see this as standard in the states and we will all make sure it becomes standard here. Over the next couple of weeks, I will re-design the curriculum and figure out ways to implement the academic programs, one by one.
In the coming weeks we have a bit of complex surgery. I’ll elaborate in the blog as they come about: A teenager with a facial rhabdomyosarcoma resistant to 18 rounds of chemo, another younger teenager with squamous cell carcinoma of the neck lymph nodes with an unknown primary, our myoepithelial carcinoma with a pec flap and the oropharyngeal hematoma. Mixed into this time, I will also need to fly to Addis to finish my standard paperwork for my contract (which takes 3 days). There was a time in the past couple of weeks when I wasn’t sure if I would have enough to do here. Its clear now that the opposite issue is much more likely.





One thought on “My worst nightmare continues…”